Insights
Sepsis forces clinicians to make extremely difficult choices

If you find yourself in a hospital bed, there are reasons for optimism. You are in the hands of healthcare professionals who will almost certainly have cared for countless other patients facing the same medical condition as you. Your treatment is guided by scientific foundations, protocols, and the real-world experience of doctors, nurses and other healthcare staff.
But it can be easy to take quality healthcare for granted. Behind the clinical veneer, it is ultimately people who are making decisions to make you better. Antibiotics? Ventilator? Emergency operation? Often these choices are made at speed, with incomplete information, by exhausted healthcare workers at the end of long shifts. Despite their heroics, medical staff are only human and ICU workers are suffering from stress and burnout exacerbated by the COVID-19 pandemic.
Sepsis – blood poisoning caused by bacteria – presents a particularly challenging scenario for healthcare workers. When sepsis strikes, an otherwise healthy patient can deteriorate into a life-threatening situation within hours. Left untreated, sepsis has a mortality rate of 30–50% so speed is essential. Under the UK’s National Early Warning Score (NEWS2) system, all patients receive physiological checks upon hospital admission, repeated at least every 12 hours. Respiration rate, oxygen saturation and signs of confusion are among the factors assessed; if a patient’s cumulative score crosses a threshold, a clinician is alerted.
Difficult decisions
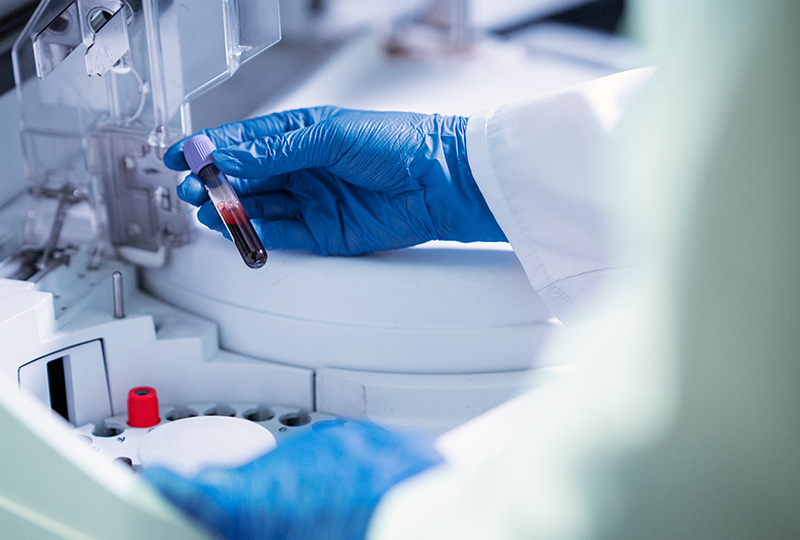
At that point, a patient may be rushed onto the Sepsis Six pathway, or similar protocol depending on the healthcare system. Blood samples are taken to the lab for a blood culturing process to confirm:
- Is bacteria present?
- If so, what is it?
- What is the bacteria’s resistance to different antibiotics?
As this process takes several days, patients are given broad-spectrum IV antibiotics in the meantime: often a blend of amoxicillin, azithromycin and gentamicin. While necessary, this treatment can have nasty side effects, including wiping out the gut microbiome and long-term damage to liver and kidney function. For medical practitioners, the decision to administer IV antibiotics – knowing that in hindsight they may turn out to be unnecessary – can be especially difficult in the case of neonates. But given the risks, the alternative of doing nothing is simply not an option.
Worldwide, one in five deaths is attributable to sepsis. It is the leading cause of in-hospital deaths in the US and has a particularly high burden in sub-Saharan Africa, Oceania, and parts of Asia. Everywhere, sepsis places strain on medical practitioners far beyond the ICU team. Survivors often require ongoing support from physios, dieticians, nurses and a range of other specialists who deal with the consequence of damage to vital organs.
What’s more, the way we treat sepsis is also locked in a vicious cycle with the problem of antimicrobial resistance (AMR). Historic overuse (or patient misuse) of antibiotics in medicine and agriculture is leading to pathogens that are increasingly resistant to our antibiotics. In 2019, 1.27 million deaths were directly attributable to AMR and the problem may have been exacerbated by the prophylactic (precautionary), yet understandable, use of antibiotics in COVID-19 patients.
AMR threatens the foundations of modern medicine
The threat of AMR to our healthcare paradigm cannot be overstated. It is already forcing healthcare workers to change their practices. In 20% of cases in the UK where frontline antibiotics are used they are no longer effective, and that figure is significantly higher in some other countries. Antibiotics are essential to many procedures, from surgery to childbirth and cancer treatment, and no new antibiotic classes have been discovered since the 1980s. If vulnerable patients can no longer rely on existing antibiotics, the consequences are catastrophic. Also, routine procedures such as hip replacements may no longer be worth the risk, with far-reaching consequences for wellbeing and community support services.
Fortunately, governments and international organisations have recognised the need to tackle the AMR issue. In 2015 the World Healthcare Organization launched a Global Action Plan to tackle AMR (GAP-AMR) and established the Global Antimicrobial Resistance and Use Surveillance System (GLASS). Global consortia such as CARB-X are supporting research innovations and emerging technologies. And the UK is one of more than 150 countries to develop an AMR national action plan, which includes providing support for innovative ways to prevent and control infections.
At GenomeKey, we are tackling the dual threat of sepsis and AMR head on. We have developed a rapid data-driven IVD device that can identify sepsis-causing bacteria within hours. By replacing blood cultures with a genome sequencing technique, we are able to provide life-saving information faster and more reliably.